
Supportive treatments are offered including short-term anti-emetics (long-term vestibular sedatives delay compensation). The HINTS examination (Supplementary Table 2) can be used to differentiate this from acute cerebellar strokes. VN is also sometimes incorrectly referred to as labyrinthitis - labyrinthitis by definition involves a loss of hearing as well. It is thought to be due to viruses affecting the superior vestibular nerve in its narrow bony canal. This condition classically causes debilitating sudden vertigo often following a viral upper respiratory tract infection. This examination has been shown to have 100% sensitivity and 96% specificity for stoke, 3 but does need practice and training, and only relates to acute presentations of dizziness. The HINTS examination is a useful tool to distinguish VN from cerebellar stroke (Supplementary Table 2).
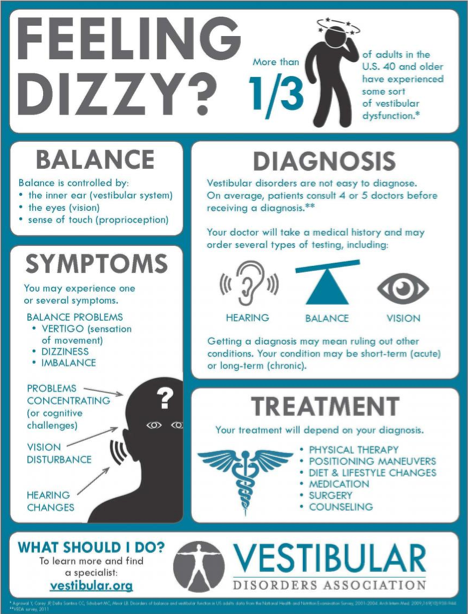
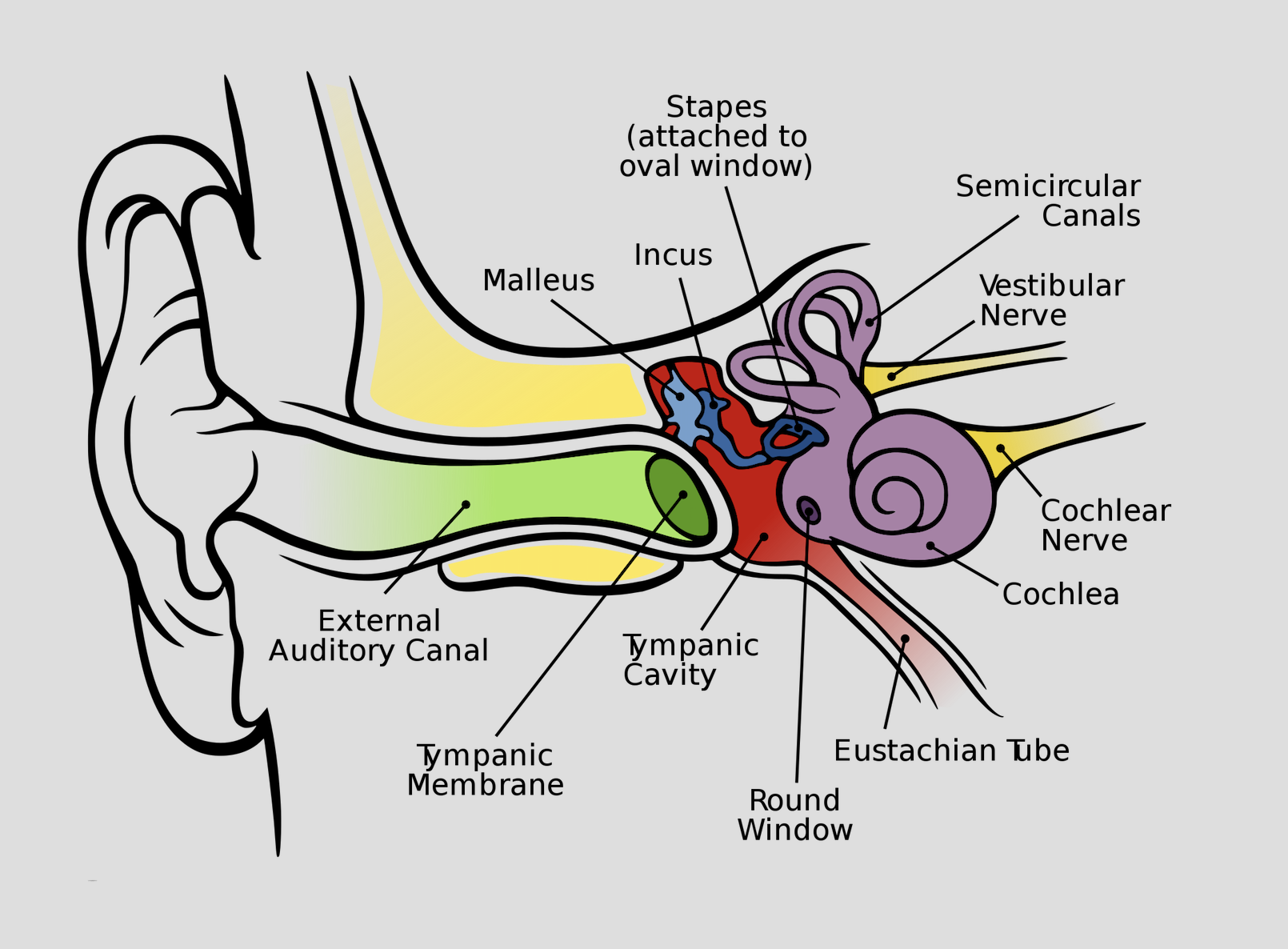
AICA strokes in particular can also cause hearing loss. The main concern here is not missing a cerebellar vascular event involving the anterior or posterior inferior cerebellar arteries (AICA or PICA respectively), which can mimic VN. Presence of geotropic (beating towards the ground), torsional nystagmus on Dix–Hallpike testing supports a diagnosis of BPPV and can be followed by a therapeutic Epley manoeuvre. Dix–Hallpike testing can be used to diagnose BPPV. A detailed history (Supplementary Table 1) can diagnose the majority of both vestibular and non-vestibular causes.Ī detailed neuro-otological examination should be undertaken including otoscopy, cranial nerve examination, HINTS examination (Supplementary Table 2), Romberg’s (test of proprioception and dorsal column function) and Unterberger’s test (as per Romberg’s but with the patient marching on the spot, rotating towards side of vestibular hypofunction), and a lying and standing blood pressure reading.


 0 kommentar(er)
0 kommentar(er)
